
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Rheumatoid Arthritis in the Feet
Rheumatoid Arthritis is a chronic progressive disease that attacks several joints throughout the body. It is an autoimmune disease in which the body’s immune system mistakenly attacks the joints. As a result, the tissue inside the joints, called synovium, starts to thicken and causes pain around the joints. The synovium is responsible for creating a fluid that lubricates the joints to help them move. Approximately 1.5 million people in the United States have Rheumatoid Arthritis. Women are almost three times as likely to have RA compared to men, and it’s disease usually begins between the ages of 30 and 60. People who have a genetic history of RA are more likely to develop the disease.
Symptoms of RA may include the following sensations in the joints: pain, tenderness, swelling, redness, warmth, stiffness, and loss of range. Swollen joints are a very common symptom for those with the disease. At times, it may be minimal, but it may also be very apparent. Another typical symptom is joint stiffness. Doctors will often use the direction of morning stiffness to measure the severity of a patient’s joint inflammation. Other RA symptoms include limping, anemia, fever, and fatigue.
To diagnose RA, your podiatrist will typically request x-rays to see how much damage there is in the joints. Blood tests may also be performed to show if there are any signs of anemia, or antibodies such as the rheumatoid factor. If you have previously been diagnosed with RA, you should know the disease may spread to your feet and ankles.
There are many non-surgical options that can be used to treat this ailment. Some of these options include physical therapy, foot massages, orthotics, bracing, supportive shoes, and steroid injections. Physical therapy is useful because it will help stretch and strengthen the joints in both the foot and ankle to improve joint function. Massages can help improve blood circulation which will be good for the feet. Choosing proper footwear will allow you to walk with comfortability if you are a sufferer from RA. Lastly, bracing will help stabilize the foot joints, limit deformities and decrease pain.
In severe cases, surgery may be a treatment option that should be considered. For those who cannot walk without experiencing pain and those whose deformities can not be managed with braces, surgery should be considered. Your podiatrist will recommend surgery if he or she believes it will improve your foot biomechanics.
Diabetes and Heel Fissures

Cracked heels, or heel fissures, are cracks or splits in the skin on the soles of the feet, often going through to the inner layers of skin. They can be painful when pressure is applied to the skin while standing, and they can bleed. This condition generally comes from dry skin. Loss of nerve supply to the sweat glands in the feet can happen to diabetics, because they tend to have drier skin than others. Heel fissures are common in the general population, but those with diabetes can have more serious consequences if they do not deal with cracked heels effectively. Diabetics can also suffer from neuropathy, causing loss of feeling in the feet. With the loss of sensation, patients with diabetes can have fissures that bleed and can possibly become infected and ulcerated without knowing it. If you are a diabetic, make sure to visually inspect your feet regularly. If you have cracked heels or some other foot problem, it is important for you to see a podiatrist for prompt treatment.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Anna Petrov from Family Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Wheeling and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
Obesity and Foot Swelling

Having swollen feet is certainly not a pleasant experience. Swelling in the feet occurs when bodily fluids become trapped or built-up in the tissues. As a result, the affected area can become significantly puffy, causing them to look markedly bigger than usual. Although swelling in the feet has a litany of different causes, obesity is one potential contributing factor to swollen feet. When an individual is obese, or overweight, they can sometimes experience reduced blood circulation, which then can make the feet become swollen. Additionally, since obese people carry more weight, they consequently exert more pressure on their feet and this can cause pain when walking. As a result, obese people may minimize their physical activity, which can make fluids become trapped in the feet. If you are an individual that struggles with obesity, please schedule an appointment with a podiatrist to discuss ways to mitigate your foot pain. In consultation with your podiatrist, you may discuss whether or not losing weight would help you reduce the problems that you are experiencing in your feet. Do not take any chances with the health of your feet–contact a podiatrist today.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Dr. Anna Petrov from Family Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions please feel free to contact one of our offices located in Wheeling and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Obesity and the Feet
Obesity is a common problem in American society. Approximately one third of the U.S. population is obese. Obesity is defined as a body mass index greater than 30. Obesity has the power to affect different aspects of the body, and one of the most common problems it causes is foot pain. There have been many studies that found a connection between an increased BMI and foot problems. A simple activity such as walking up a flight of stairs can increase pressure on the ankle by four to six times.
Being overweight causes the body to compensate for the extra weight by changing the way it moves. Consequently, people who struggle with obesity commonly have arch problems in their feet. Obesity causes the arch to break by stretching the ligaments and tendons that hold the bones in the foot together. When the arch lowers, the foot may eventually fall flat. Collapsed foot arches fail to provide adequate shock absorption which eventually leads to foot pain. Other conditions that may be caused by flat feet are pronation, plantar fasciitis, weak ankles, and shin splints.
Foot problems that are caused by obesity may be treated by wearing proper footwear. Proper shoes will allow your feet to have better circulation around the arch and ankle. Additionally, those with obesity often discover that typical heel pain remedies are not effective for them. They will find that their plantar fascia is easily injured, and it is often inflamed. The best way to treat this problem is to implement lifestyle changes. A few good ways to improve your diet are to reduce calories, fill up on fruits and veggies, and to limit sugars.
Custom foot orthotics can prevent foot problems if you’re carrying excess weight or are trying to lose weight. The purpose of orthotics is to provide shock absorption to decrease the amount of stress on the joints to prevent arthritis.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
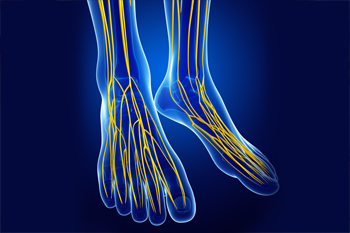
Pinched Nerves Can Cause a Variety of Uncomfortable Symptoms
A pinched, or compressed, nerve can occur anywhere in your foot, such as in the heel, ball, or even on the bottom. A pinched nerve can produce pain or sensations of tingling, numbness, weakness, or the feeling that your foot has fallen asleep. The pain may radiate out to the toes or arches and become noticeable after exercising, walking, or standing for a while. What causes a nerve in your foot to become pinched? Injuries, medical conditions, tight ligaments, inflamed tendons, wearing tight shoes, obesity, or nerve entrapment conditions such as Morton’s neuroma. Switching footwear, resting, icing, immobilizing the area, or massaging it can sometimes provide temporary relief. However, if the symptoms persist or worsen, a podiatrist should examine your foot and run tests to determine the cause of your condition. Taking prompt, appropriate action will help reduce the risk of permanent nerve damage.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Anna Petrov from Family Foot & Ankle Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in Wheeling and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.












